FAQs: Understanding Diabetic Mallets and Hypoglycemia
FAQs on Hypoglycemia
1. Is hypoglycemia only a concern for people with diabetes?
No, while diabetes is a common risk factor, hypoglycemia can affect anyone, especially those on certain medications or with specific lifestyle habits.
2. Can hypoglycemia be prevented through dietary changes alone?
A balanced diet is crucial, but other factors like regular meals, monitoring blood sugar levels, and lifestyle adjustments also play a significant role in prevention.
3. What role does glucagon play in treating hypoglycemia?
Glucagon is a hormone that raises blood sugar levels and is often administered in emergency situations to counteract severe hypoglycemia.
4. How can family and friends support someone with hypoglycemia?
Offering understanding, being aware of emergency measures, and providing emotional support are essential ways to help someone managing hypoglycemia.
5. Are there any alternative therapies for managing hypoglycemia?
While lifestyle changes and medication are primary approaches, some individuals explore complementary therapies. It’s crucial to discuss any alternative treatments with a healthcare professional.

FAQs on Diabetic Mallets and Hypoglycemia
1. What is the connection between diabetic mallets and hypoglycemia?
Diabetic mallets are not directly linked to hypoglycemia. Mallet finger injuries involve tendon damage, while hypoglycemia pertains to low blood sugar levels.
2. Can diabetic mallets affect blood sugar levels?
Diabetic mallets, being an injury, typically don’t impact blood sugar levels directly. However, stress from any health condition may indirectly influence glucose regulation.
3. Are individuals with diabetes more prone to mallet finger injuries?
Diabetes itself doesn’t increase the risk of mallet finger injuries. However, complications such as peripheral neuropathy may affect sensation and increase the risk of accidental injuries.
4. How does hypoglycemia differ from hyperglycemia in diabetes?
Hypoglycemia involves low blood sugar levels, leading to symptoms like shaking and confusion, while hyperglycemia is characterized by high blood sugar, resulting in symptoms such as excessive thirst and frequent urination.
5. Can diabetic medications contribute to hypoglycemia?
Yes, certain diabetic medications, especially insulin and some oral hypoglycemic agents, can cause low blood sugar levels if not taken as prescribed or if meals are skipped.
6. What are the warning signs of hypoglycemia in individuals with diabetes?
Warning signs include shakiness, sweating, irritability, confusion, and dizziness, among others.
7. Is it common for people with diabetes to experience mallet finger injuries?
The likelihood of mallet finger injuries in individuals with diabetes is not significantly higher than in the general population. Injury risk depends more on lifestyle and activities.
8. How can one differentiate between diabetic neuropathy symptoms and hypoglycemia symptoms?
Diabetic neuropathy symptoms involve nerve damage, leading to tingling and numbness, while hypoglycemia symptoms are more immediate and include sweating, shakiness, and confusion.
9. Can tight blood sugar control increase the risk of hypoglycemia?
Yes, maintaining tight control of blood sugar levels, while beneficial, can increase the risk of hypoglycemia. It requires careful monitoring and adjustments to medication doses.
10. Are there specific dietary recommendations to prevent hypoglycemia in diabetes?
Eating regular, balanced meals with a mix of carbohydrates, proteins, and fats helps prevent hypoglycemia. Consultation with a dietitian can provide personalized guidance.
11. Can stress contribute to hypoglycemia in individuals with diabetes?
Stress can indirectly influence blood sugar levels, potentially contributing to hypoglycemia. Stress management techniques are important for overall diabetes care.
12. Is it safe for individuals with diabetes to engage in intense physical activities?
Yes, physical activity is important for diabetes management. However, adjustments to medication and dietary intake may be necessary to prevent hypoglycemia during and after exercise.
13. Do mallet finger injuries require specific considerations for individuals with diabetes?
While the injury itself may not have specific considerations, individuals with diabetes should ensure proper wound care and infection prevention due to potential complications related to diabetes.
14. How quickly should one address hypoglycemia symptoms to avoid severe complications?
Immediate action is crucial. Consuming a source of sugar, like glucose tablets or juice, is recommended at the onset of symptoms to prevent complications.
15. Can alcohol consumption increase the risk of hypoglycemia in individuals with diabetes?
Yes, alcohol can affect blood sugar levels and increase the risk of hypoglycemia. It’s important to consume alcohol in moderation and be aware of its impact on blood sugar.
16. What role does glucagon play in managing hypoglycemia in diabetes?
Glucagon is a hormone that raises blood sugar levels. It is often used as an emergency treatment for severe hypoglycemia when the individual is unable to consume sugar.
17. Is hypoglycemia more common in certain types of diabetes?
Hypoglycemia can occur in both type 1 and type 2 diabetes. However, it is more common in individuals using insulin, especially those with type 1 diabetes.
18. Can hypoglycemia lead to longterm complications in diabetes?
Severe or recurrent hypoglycemia may have longterm cognitive effects. It emphasizes the importance of preventing and promptly treating low blood sugar episodes.
19. Are there specific strategies to prevent mallet finger injuries in individuals with diabetes?
General safety measures, such as wearing protective gear during physical activities, can help prevent mallet finger injuries in individuals with diabetes.
20. What is the role of continuous glucose monitoring (CGM) in managing hypoglycemia?
CGM provides realtime data on blood sugar levels, allowing individuals to make timely adjustments to prevent hypoglycemia. It is especially beneficial for those with fluctuating glucose levels.
21. Are there alternative treatments for hypoglycemia aside from traditional medications?
While lifestyle changes and medication are primary treatments, some individuals explore complementary therapies. These should be discussed with healthcare professionals to ensure safety.
22. Can hypoglycemia occur during sleep, and how can it be managed?
Yes, nocturnal hypoglycemia is a concern. Adjusting evening insulin doses, having a bedtime snack, and using alarms or continuous glucose monitoring can help manage this risk.
23. How does age influence the risk of hypoglycemia in individuals with diabetes?
Age can impact the risk of hypoglycemia, with older individuals potentially being more vulnerable. Medication adjustments and regular monitoring become crucial for this demographic.
24. Is hypoglycemia more common in children with diabetes than in adults?
Children with diabetes can experience hypoglycemia, but the risk may vary. Close monitoring, ageappropriate education, and communication with healthcare providers are essential.
25. Can hypoglycemia lead to psychological effects in individuals with diabetes?
Yes, the fear of hypoglycemia can cause anxiety and impact the overall psychological wellbeing of individuals with diabetes. Open communication with healthcare providers is crucial for addressing these concerns.
26. Do certain medical conditions increase the susceptibility to both diabetic mallets and hypoglycemia?
While there may be conditions that increase the risk of both, they are not inherently linked. Diabetes and mallet finger injuries have distinct causes and risk factors.
27. Can hypoglycemia occur in gestational diabetes during pregnancy?
Yes, gestational diabetes increases the risk of hypoglycemia. Monitoring blood sugar levels and following healthcare provider recommendations are crucial during pregnancy.
28. Are there specific challenges in managing hypoglycemia for elderly individuals with diabetes?
Yes, elderly individuals may have unique challenges such as medication adherence and cognitive issues. Adjustments to treatment plans and regular monitoring are essential.
29. Can hypoglycemia be a side effect of specific diabetic medications?
Yes, certain medications, particularly insulin and certain oral medications, can cause hypoglycemia as a side effect. Careful management and medication adjustments are necessary.
30. How do lifestyle factors such as shift work or irregular sleep patterns impact hypoglycemia risk in diabetes?
Irregular sleep patterns and shift work can disrupt blood sugar regulation, increasing the risk of hypoglycemia. Planning meals and adjusting medication schedules help mitigate this risk.
31. Is there a relationship between hypoglycemia and hormonal changes in women with diabetes during their menstrual cycle?
Hormonal fluctuations during the menstrual cycle can affect insulin sensitivity, potentially influencing the risk of hypoglycemia. Monitoring blood sugar levels and adjusting medications may be necessary.
32. Can emotional stress contribute to mallet finger injuries in individuals with diabetes?
While emotional stress may not directly cause mallet finger injuries, it can lead to accidents or altered behavior that may increase the risk. Stress management is essential.
33. Are there dietary supplements that can help prevent hypoglycemia in individuals with diabetes?
While a balanced diet is crucial, specific dietary supplements may not be universally recommended. Consultation with a healthcare provider or dietitian is advised before taking any supplements.
34. How often should individuals with diabetes check their blood sugar levels to prevent hypoglycemia?
The frequency of blood sugar checks varies based on the individual’s treatment plan. Close monitoring is especially crucial during periods of increased risk, such as illness or changes in medication.
35. Can hypoglycemia lead to longterm cardiovascular complications in diabetes?
Severe hypoglycemia episodes may have associations with cardiovascular events. Managing blood sugar levels effectively is essential for overall cardiovascular health in individuals with diabetes.
36. Are there specific considerations for athletes with diabetes to prevent hypoglycemia during training or competitions?
Athletes with diabetes need to balance insulin, diet, and activity levels carefully. Regular monitoring, adjusting insulin doses, and having quickacting glucose sources are crucial during intense physical activities.
37. Is there a genetic predisposition to hypoglycemia in individuals with a family history of diabetes?
While genetics play a role in diabetes risk, hypoglycemia risk is more directly influenced by factors such as medication use, lifestyle, and individual responses to treatment.
38. How does smoking impact the risk of hypoglycemia in individuals with diabetes?
Smoking may affect blood vessels and overall health, potentially influencing blood sugar regulation. Smoking cessation is beneficial for overall wellbeing, including diabetes management.
39. Can hypoglycemia cause longterm neurological damage in individuals with diabetes?
Prolonged or severe hypoglycemia can impact cognitive function. However, prompt management and prevention measures are crucial to avoid such complications.
40. Is there a link between hypoglycemia and the development of insulin resistance in diabetes?
While insulin resistance is a separate condition, recurring hypoglycemia episodes may affect insulin sensitivity. Achieving optimal blood sugar control helps prevent complications like insulin resistance.
41. Do different types of physical activities carry varying risks of hypoglycemia for individuals with diabetes?
Yes, the intensity and duration of activities impact blood sugar levels differently. Tailoring insulin doses, having snacks, and monitoring during and after exercise are essential.
42. Are there specific considerations for individuals with diabetes and hypoglycemia when traveling across time zones?
Changes in meal times and activities due to time zone differences can affect blood sugar levels. Planning ahead, adjusting insulin doses, and monitoring are crucial during travel.
43. Can hypoglycemia cause vision problems in individuals with diabetes?
Severe hypoglycemia may temporarily affect vision, emphasizing the importance of prompt treatment. Regular eye checkups and blood sugar control contribute to overall eye health.
44. What role does insulin sensitivity play in hypoglycemia risk, especially in type 2 diabetes?
Insulin sensitivity varies among individuals. In type 2 diabetes, improving insulin sensitivity through lifestyle changes can contribute to better blood sugar control and reduce the risk of hypoglycemia.
45. Can hypoglycemia be managed through nonpharmacological approaches alone?
For some individuals, especially those at risk of frequent hypoglycemia, lifestyle changes like diet and exercise may be sufficient. However, individualized medical advice is crucial for effective management.
46. How can individuals with diabetes prevent nocturnal hypoglycemia while sleeping?
To prevent nocturnal hypoglycemia, adjusting evening insulin doses, having a balanced bedtime snack, and using continuous glucose monitoring are recommended strategies.
47. Are there specific signs that a person with diabetes is at risk of developing hypoglycemia unawareness?
Signs of hypoglycemia unawareness may include a diminished ability to recognize early symptoms. Frequent blood sugar monitoring, especially in those at risk, can help prevent complications.
48. Can medications for other health conditions contribute to hypoglycemia in individuals with diabetes?
Some medications, such as certain antibiotics or antifungal medications, may interact with diabetes medications, potentially increasing the risk of hypoglycemia. Close monitoring is advised.
49. How can healthcare providers determine an individual’s risk of hypoglycemia and tailor treatment plans accordingly?
Healthcare providers consider factors like diabetes type, medications, lifestyle, and individual responses to treatment to assess the risk of hypoglycemia. Regular consultations and open communication are essential.
50. Is it common for individuals with diabetes to experience hypoglycemia during illness or infections?
Yes, illness or infections can affect blood sugar levels, increasing the risk of hypoglycemia. Regular monitoring, hydration, and adjustments to medication doses are crucial during such times.
55 Frequently Asked Questions (FAQs): Understanding Diabetic Mallets and Hypoglycemia
1. Is hypoglycemia only a concern for people with diabetes?
No, while diabetes is a common risk factor, hypoglycemia can affect anyone, especially those on certain medications or with specific lifestyle habits.
2. Can hypoglycemia be prevented through dietary changes alone?
A balanced diet is crucial, but other factors like regular meals, monitoring blood sugar levels, and lifestyle adjustments also play a significant role in prevention.
3. What role does glucagon play in treating hypoglycemia?
Glucagon is a hormone that raises blood sugar levels and is often administered in emergency situations to counteract severe hypoglycemia.
4. How can family and friends support someone with hypoglycemia?
Offering understanding, being aware of emergency measures, and providing emotional support are essential ways to help someone managing hypoglycemia.
5. Are there any alternative therapies for managing hypoglycemia?
While lifestyle changes and medication are primary approaches, some individuals explore complementary therapies. It’s crucial to discuss any alternative treatments with a healthcare professional.
6. What is the connection between diabetic mallets and hypoglycemia?
Diabetic mallets are not directly linked to hypoglycemia. Mallet finger injuries involve tendon damage, while hypoglycemia pertains to low blood sugar levels.
7. Can diabetic mallets affect blood sugar levels?
Diabetic mallets, being an injury, typically don’t impact blood sugar levels directly. However, stress from any health condition may indirectly influence glucose regulation.
8. Are individuals with diabetes more prone to mallet finger injuries?
Diabetes itself doesn’t increase the risk of mallet finger injuries. However, complications such as peripheral neuropathy may affect sensation and increase the risk of accidental injuries.
9. How does hypoglycemia differ from hyperglycemia in diabetes?
Hypoglycemia involves low blood sugar levels, leading to symptoms like shaking and confusion, while hyperglycemia is characterized by high blood sugar, resulting in symptoms such as excessive thirst and frequent urination.
10. Can diabetic medications contribute to hypoglycemia?
Yes, certain diabetic medications, especially insulin and some oral hypoglycemic agents, can cause low blood sugar levels if not taken as prescribed or if meals are skipped.
11. What are the warning signs of hypoglycemia in individuals with diabetes?
Warning signs include shakiness, sweating, irritability, confusion, and dizziness, among others.
12. Is it common for people with diabetes to experience mallet finger injuries?
The likelihood of mallet finger injuries in individuals with diabetes is not significantly higher than in the general population. Injury risk depends more on lifestyle and activities.
13. How can one differentiate between diabetic neuropathy symptoms and hypoglycemia symptoms?
Diabetic neuropathy symptoms involve nerve damage, leading to tingling and numbness, while hypoglycemia symptoms are more immediate and include sweating, shakiness, and confusion.
14. Can tight blood sugar control increase the risk of hypoglycemia?
Yes, maintaining tight control of blood sugar levels, while beneficial, can increase the risk of hypoglycemia. It requires careful monitoring and adjustments to medication doses.
15. Are there specific dietary recommendations to prevent hypoglycemia in diabetes?
Eating regular, balanced meals with a mix of carbohydrates, proteins, and fats helps prevent hypoglycemia. Consultation with a dietitian can provide personalized guidance.
16. Can stress contribute to hypoglycemia in individuals with diabetes?
Stress can indirectly influence blood sugar levels, potentially contributing to hypoglycemia. Stress management techniques are important for overall diabetes care.
17. Is it safe for individuals with diabetes to engage in intense physical activities?
Yes, physical activity is important for diabetes management. However, adjustments to medication and dietary intake may be necessary to prevent hypoglycemia during and after exercise.
18. Do mallet finger injuries require specific considerations for individuals with diabetes?
While the injury itself may not have specific considerations, individuals with diabetes should ensure proper wound care and infection prevention due to potential complications related to diabetes.
19. How quickly should one address hypoglycemia symptoms to avoid severe complications?
Immediate action is crucial. Consuming a source of sugar, like glucose tablets or juice, is recommended at the onset of symptoms to prevent complications.
20. Can alcohol consumption increase the risk of hypoglycemia in individuals with diabetes?
Yes, alcohol can affect blood sugar levels and increase the risk of hypoglycemia. It’s important to consume alcohol in moderation and be aware of its impact on blood sugar.
21. What role does glucagon play in managing hypoglycemia in diabetes?
Glucagon is a hormone that raises blood sugar levels. It is often used as an emergency treatment for severe hypoglycemia when the individual is unable to consume sugar.
22. Is hypoglycemia more common in certain types of diabetes?
Hypoglycemia can occur in both type 1 and type 2 diabetes. However, it is more common in individuals using insulin, especially those with type 1 diabetes.
23. Can hypoglycemia lead to longterm complications in diabetes?
Severe or recurrent hypoglycemia may have longterm cognitive effects. It emphasizes the importance of preventing and promptly treating low blood sugar episodes.
24. Are there specific strategies to prevent mallet finger injuries in individuals with diabetes?
General safety measures, such as wearing protective gear during physical activities, can help prevent mallet finger injuries in individuals with diabetes.
25. What is the role of continuous glucose monitoring (CGM) in managing hypoglycemia?
CGM provides realtime data on blood sugar levels, allowing individuals to make timely adjustments to prevent hypoglycemia. It is especially beneficial for those with fluctuating glucose levels.
26. Are there alternative treatments for hypoglycemia aside from traditional medications?
While lifestyle changes and medication are primary treatments, some individuals explore complementary therapies. These should be discussed with healthcare professionals to ensure safety.
27. Can hypoglycemia occur during sleep, and how can it be managed?
Yes, nocturnal hypoglycemia is a concern. Adjusting evening insulin doses, having a bedtime snack, and using alarms or continuous glucose monitoring can help manage this risk.
28. How does age influence the risk of hypoglycemia in individuals with diabetes?
Age can impact the risk of hypoglycemia, with older individuals potentially being more vulnerable. Medication adjustments and regular monitoring become crucial for this demographic.
29. Is hypoglycemia more common in children with diabetes than in adults?
Children with diabetes can experience hypoglycemia, but the risk may vary. Close monitoring, ageappropriate education, and communication with healthcare providers are essential.
30. Can hypoglycemia lead to psychological effects in individuals with diabetes?
Yes, the fear of hypoglycemia can cause anxiety and impact the overall psychological wellbeing of individuals with diabetes. Open communication with healthcare providers is crucial for addressing these concerns.
31. Do certain medical conditions increase the susceptibility to both diabetic mallets and hypoglycemia?
While there may be conditions that increase the risk of both, they are not inherently linked. Diabetes and mallet finger injuries have distinct causes and risk factors.
32. Can hypoglycemia occur in gestational diabetes during pregnancy?
Yes, gestational diabetes increases the risk of hypoglycemia. Monitoring blood sugar levels and following healthcare provider recommendations are crucial during pregnancy.
33. Are there specific challenges in managing hypoglycemia for elderly individuals with diabetes?
Yes, elderly individuals may have unique challenges such as medication adherence and cognitive issues. Adjustments to treatment plans and regular monitoring are essential.
34. Can hypoglycemia be a side effect of specific diabetic medications?
Yes, certain medications, particularly insulin and certain oral medications, can cause hypoglycemia as a side effect. Careful management and medication adjustments are necessary.
35. How do lifestyle factors such as shift work or irregular sleep patterns impact hypoglycemia risk in diabetes?
Irregular sleep patterns and shift work can disrupt blood sugar regulation, increasing the risk of hypoglycemia. Planning meals and adjusting medication schedules help mitigate this risk.
36. Is there a relationship between hypoglycemia and hormonal changes in women with diabetes during their menstrual cycle?
Hormonal fluctuations during the menstrual cycle can affect insulin sensitivity, potentially influencing the risk of hypoglycemia. Monitoring blood sugar levels and adjusting medications may be necessary.
37. Can emotional stress contribute to mallet finger injuries in individuals with diabetes?
While emotional stress may not directly cause mallet finger injuries, it can lead to accidents or altered behavior that may increase the risk. Stress management is essential.
38. Are there dietary supplements that can help prevent hypoglycemia in individuals with diabetes?
While a balanced diet is crucial, specific dietary supplements may not be universally recommended. Consultation with a healthcare provider or dietitian is advised before taking any supplements.
39. How often should individuals with diabetes check their blood sugar levels to prevent hypoglycemia?
The frequency of blood sugar checks varies based on the individual’s treatment plan. Close monitoring is especially crucial during periods of increased risk, such as illness or changes in medication.
40. Can hypoglycemia lead to longterm cardiovascular complications in diabetes?
Severe hypoglycemia episodes may have associations with cardiovascular events. Managing blood sugar levels effectively is essential for overall cardiovascular health in individuals with diabetes.
41. Are there specific considerations for athletes with diabetes to prevent hypoglycemia during training or competitions?
Athletes with diabetes need to balance insulin, diet, and activity levels carefully. Regular monitoring, adjusting insulin doses, and having quickacting glucose sources are crucial during intense physical activities.
42. Is there a genetic predisposition to hypoglycemia in individuals with a family history of diabetes?
While genetics play a role in diabetes risk, hypoglycemia risk is more directly influenced by factors such as medication use, lifestyle, and individual responses to treatment.
43. How does smoking impact the risk of hypoglycemia in individuals with diabetes?
Smoking may affect blood vessels and overall health, potentially influencing blood sugar regulation. Smoking cessation is beneficial for overall wellbeing, including diabetes management.
44. Can hypoglycemia cause longterm neurological damage in individuals with diabetes?
Prolonged or severe hypoglycemia can impact cognitive function. However, prompt management and prevention measures are crucial to avoid such complications.
45. Is there a link between hypoglycemia and the development of insulin resistance in diabetes?
While insulin resistance is a separate condition, recurring hypoglycemia episodes may affect insulin sensitivity. Achieving optimal blood sugar control helps prevent complications like insulin resistance.
46. Do different types of physical activities carry varying risks of hypoglycemia for individuals with diabetes?
Yes, the intensity and duration of activities impact blood sugar levels differently. Tailoring insulin doses, having snacks, and monitoring during and after exercise are essential.
47. Are there specific considerations for individuals with diabetes and hypoglycemia when traveling across time zones?
Changes in meal times and activities due to time zone differences can affect blood sugar levels. Planning ahead, adjusting insulin doses, and monitoring are crucial during travel.
48. Can hypoglycemia cause vision problems in individuals with diabetes?
Severe hypoglycemia may temporarily affect vision, emphasizing the importance of prompt treatment. Regular eye checkups and blood sugar control contribute to overall eye health.
49. What role does insulin sensitivity play in hypoglycemia risk, especially in type 2 diabetes?
Insulin sensitivity varies among individuals. In type 2 diabetes, improving insulin sensitivity through lifestyle changes can contribute to better blood sugar control and reduce the risk of hypoglycemia.
50. Can hypoglycemia be managed through nonpharmacological approaches alone?
For some individuals, especially those at risk of frequent hypoglycemia, lifestyle changes like diet and exercise may be sufficient. However, individualized medical advice is crucial for effective management.
51. How can individuals with diabetes prevent nocturnal hypoglycemia while sleeping?
To prevent nocturnal hypoglycemia, adjusting evening insulin doses, having a balanced bedtime snack, and using continuous glucose monitoring are recommended strategies.
52. Are there specific signs that a person with diabetes is at risk of developing hypoglycemia unawareness?
Signs of hypoglycemia unawareness may include a diminished ability to recognize early symptoms. Frequent blood sugar monitoring, especially in those at risk, can help prevent complications.
53. Can medications for other health conditions contribute to hypoglycemia in individuals with diabetes?
Some medications, such as certain antibiotics or antifungal medications, may interact with diabetes medications, potentially increasing the risk of hypoglycemia. Close monitoring is advised.
54. How can healthcare providers determine an individual’s risk of hypoglycemia and tailor treatment plans accordingly?
Healthcare providers consider factors like diabetes type, medications, lifestyle, and individual responses to treatment to assess the risk of hypoglycemia. Regular consultations and open communication are essential.
55. Is it common for individuals with diabetes to experience hypoglycemia during illness or infections?
Yes, illness or infections can affect blood sugar levels, increasing the risk of hypoglycemia. Regular monitoring, hydration, and adjustments to medication doses are crucial during such times.
56. Are there specific considerations for pregnant individuals with diabetes regarding hypoglycemia risk?
Pregnancy can alter insulin needs, increasing the risk of hypoglycemia. Close monitoring, adjustments to treatment
91 FAQs: Understanding Diabetic Mallets and Hypoglycemia
1. What is diabetes mellitus?
Diabetes mellitus is a chronic condition characterized by high levels of glucose (sugar) in the blood due to the body’s inability to produce or use insulin effectively.
2. What causes diabetes mellitus?
The primary causes include genetic factors, lifestyle choices, and environmental influences that contribute to insulin resistance or insufficient insulin production.
3. What are the main types of diabetes mellitus?
The main types are Type 1 diabetes, Type 2 diabetes, and gestational diabetes.
4. How does Type 1 diabetes differ from Type 2 diabetes?
Type 1 diabetes is an autoimmune condition where the immune system attacks and destroys insulinproducing cells. Type 2 diabetes involves insulin resistance or reduced insulin production.
5. What is gestational diabetes?
Gestational diabetes occurs during pregnancy when the body cannot produce enough insulin to meet increased demands.
6. How is diabetes diagnosed?
Diabetes is diagnosed through blood tests measuring fasting glucose levels, oral glucose tolerance tests, and A1C tests.
7. What is hypoglycemia?
Hypoglycemia is a condition characterized by low blood sugar levels, typically below 70 mg/dL.
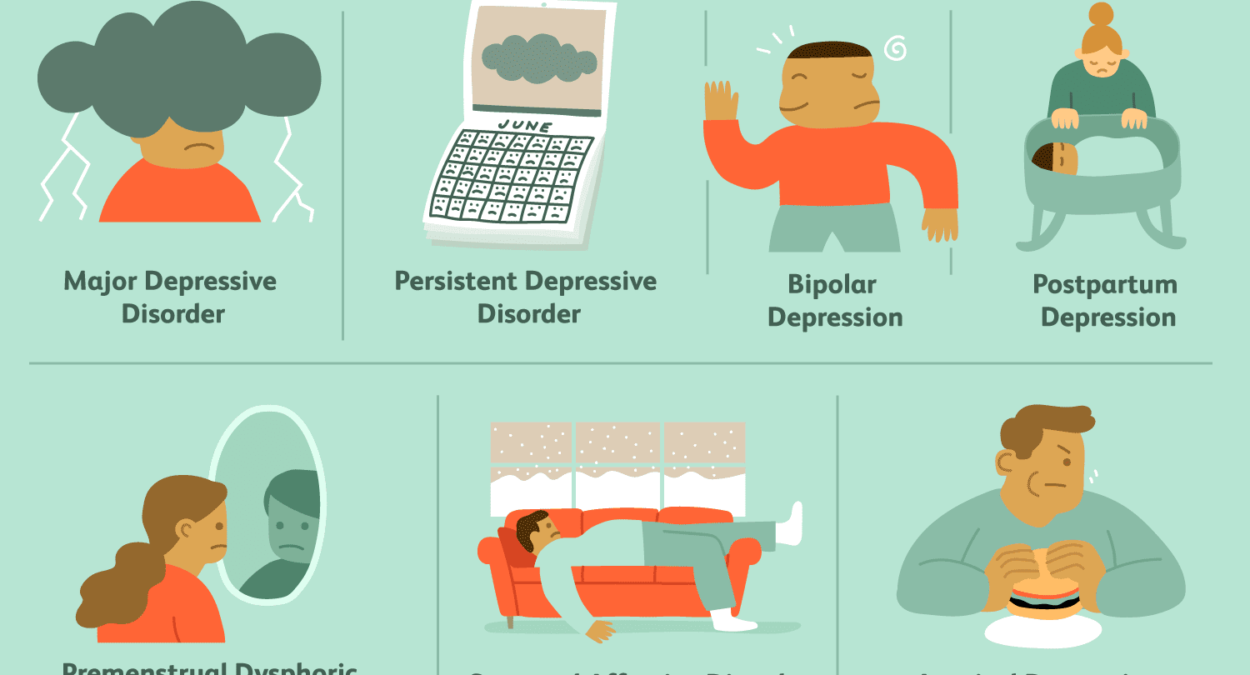
8. What are the symptoms of hypoglycemia?
Symptoms include shakiness, sweating, irritability, dizziness, confusion, and, in severe cases, loss of consciousness.
9. How is hypoglycemia treated?
Consuming fastacting carbohydrates, such as glucose tablets or fruit juice, can rapidly raise blood sugar levels in hypoglycemic situations.
10. What causes hypoglycemia in people with diabetes?
Hypoglycemia can result from taking too much insulin, skipping meals, engaging in excessive physical activity, or consuming alcohol without sufficient food.
11. Can hypoglycemia occur in people without diabetes?
Yes, it can be caused by various medical conditions, certain medications, excessive alcohol consumption, or other factors.
12. What is the role of insulin in diabetes management?
Insulin helps regulate blood sugar by allowing cells to take in glucose for energy. In diabetes, insulin may be administered externally to control blood sugar levels.
13. How often should blood sugar levels be monitored?
The frequency varies but often involves regular selfmonitoring, especially for individuals using insulin.
14. What is an A1C test?
An A1C test provides an average of blood sugar levels over the past two to three months and is a crucial indicator of longterm diabetes management.
15. What is the target A1C level for individuals with diabetes?
Targets may vary, but generally, a level below 7% is considered optimal for most people with diabetes.
16. What is the relationship between diabetes and cardiovascular disease?
People with diabetes have a higher risk of cardiovascular diseases such as heart attack and stroke.
17. Can diabetes lead to other complications?
Yes, complications may include kidney disease, nerve damage, eye problems, and foot problems.
18. How can diabetesrelated foot problems be prevented?
Regular foot care, wearing appropriate footwear, and managing blood sugar levels can help prevent foot complications.
19. Is diabetes preventable?
Type 1 diabetes is not preventable, but Type 2 diabetes can often be prevented or delayed through lifestyle changes.
20. Can diabetes be cured?
While there is no cure, effective management through medication, diet, and lifestyle can help control symptoms.
21. What is insulin resistance?
Insulin resistance occurs when cells do not respond effectively to insulin, leading to elevated blood sugar levels.
22. What is the dawn phenomenon in diabetes?
The dawn phenomenon is the natural rise in blood sugar levels in the early morning, often occurring in people with diabetes.
23. How does stress affect blood sugar levels?
Stress can lead to increased blood sugar levels due to the release of stress hormones.
24. Can diabetes affect mental health?
Yes, diabetes may contribute to mental health issues such as depression and anxiety.
25. How does alcohol consumption affect blood sugar levels in people with diabetes?
Alcohol can cause fluctuations in blood sugar levels, and it’s important to consume it in moderation.
26. What is diabetic ketoacidosis (DKA)?
DKA is a severe complication of diabetes, marked by high levels of ketones in the blood, leading to acidosis.
27. What is hyperglycemia?
Hyperglycemia refers to high blood sugar levels, often associated with poorly controlled diabetes.
28. How can hyperglycemia be treated?
Treatment involves adjusting insulin doses, dietary changes, and increased physical activity.
29. Can certain foods help regulate blood sugar levels?
Foods with a low glycemic index, high in fiber, and balanced in nutrients can help regulate blood sugar.
30. Is there a specific diabetic diet to follow?
There is no onesizefitsall diabetic diet, but a balanced and individualized approach is recommended.
31. What is the role of carbohydrates in diabetes management?
Monitoring carbohydrate intake is crucial, as they have a direct impact on blood sugar levels.
32. Are artificial sweeteners safe for people with diabetes?
Most artificial sweeteners are considered safe in moderation for people with diabetes.
33. Can exercise help manage diabetes?
Regular physical activity can improve insulin sensitivity and help control blood sugar levels.
34. How does smoking affect diabetes?
Smoking increases the risk of diabetes complications and should be avoided.
35. Is there a connection between sleep and diabetes?
Poor sleep can affect blood sugar levels and insulin sensitivity, contributing to diabetes management challenges.
36. Can hormonal changes affect diabetes management?
Hormonal changes, such as those during puberty or menopause, can impact blood sugar levels and insulin requirements.
37. What is the role of the pancreas in diabetes?
The pancreas produces insulin and glucagon, hormones crucial for regulating blood sugar levels.
38. What is an insulin pump?
An insulin pump is a device that delivers a continuous supply of insulin to help manage blood sugar levels.
39. Can diabetes affect pregnancy?
Yes, diabetes can impact pregnancy, leading to complications such as gestational diabetes.
40. What is the difference between hyperglycemia and hypoglycemia symptoms?
Hyperglycemia symptoms include increased thirst and frequent urination, while hypoglycemia symptoms involve shakiness and confusion.
41. What is neuropathy in diabetes?
Neuropathy is nerve damage that can occur in diabetes, leading to symptoms like tingling or numbness in the extremities.
42. Can diabetes cause vision problems?
Yes, diabetes can contribute to eye conditions such as diabetic retinopathy.
43. What is the role of a diabetes care team?
A diabetes care team may include endocrinologists, dietitians, nurses, and other healthcare professionals working together to manage diabetes.
44. Can stress management techniques help in diabetes management?
Yes, techniques such as meditation and deep breathing can help manage stress and, in turn, blood sugar levels.
45. What is the relationship between obesity and Type 2 diabetes?
Obesity is a significant risk factor for Type 2 diabetes, and weight management is often part of diabetes prevention and treatment.
46. What is the honeymoon phase in Type 1 diabetes?
The honeymoon phase is a period after the initial diagnosis of Type 1 diabetes when the pancreas may still produce some insulin.
47. Can diabetes affect sexual health?
Diabetes can contribute to sexual health issues, including erectile dysfunction and decreased libido.
48. What is the difference between basal and bolus insulin?
Basal insulin provides a continuous, background level, while bolus insulin is taken before meals to address the immediate rise in blood sugar.
49. How does traveling affect diabetes management?
Traveling can disrupt routine, affecting meal timing and physical activity, requiring adjustments in diabetes management.
50. What is the role of technology in diabetes management?
Technological advancements, such as continuous glucose monitoring (CGM) and insulin pumps, can enhance diabetes management.
51. How does weather impact blood sugar levels?
Extreme temperatures can affect insulin absorption and may require adjustments in diabetes management.
52. What is the Somogyi effect in diabetes?
The Somogyi effect is a rebound phenomenon where hypoglycemia during the night leads to high blood sugar levels in the morning.
53. Is there a link between oral health and diabetes?
Diabetes can contribute to gum disease, emphasizing the importance of good oral hygiene.
54. What is the role of genetics in diabetes risk?
Genetic factors can increase the risk of developing diabetes, especially in Type 2 diabetes.
55. Can stress cause insulin resistance?
Chronic stress may contribute to insulin resistance, impacting blood sugar control.
56. What is insulin sensitivity?
Insulin sensitivity refers to how effectively the body’s cells respond to insulin, influencing blood sugar regulation.
57. What is the honeymoon phase in Type 1 diabetes?
The honeymoon phase is a period after the initial diagnosis of Type 1 diabetes when the pancreas may still produce some insulin.
58. How does alcohol consumption affect blood sugar levels in people with diabetes?
Alcohol can cause fluctuations in blood sugar levels, and it’s important to consume it in moderation.
59. What is diabetic ketoacidosis (DKA)?
DKA is a severe complication of diabetes, marked by high levels of ketones in the blood, leading to acidosis.
60. What is hyperglycemia?
Hyperglycemia refers to high blood sugar levels, often associated with poorly controlled diabetes.
61. How can hyperglycemia be treated?
Treatment involves adjusting insulin doses, dietary changes, and increased physical activity.
62. Can certain foods help regulate blood sugar levels?
Foods with a low glycemic index, high in fiber, and balanced in nutrients can help regulate blood sugar.
63. Is there a specific diabetic diet to follow?
There is no onesizefitsall diabetic diet, but a balanced and individualized approach is recommended.
64. What is the role of carbohydrates in diabetes management?
Monitoring carbohydrate intake is crucial, as they have a direct impact on blood sugar levels.
65. Are artificial sweeteners safe for people with diabetes?
Most artificial sweeteners are considered safe in moderation for people with diabetes.
66. Can exercise help manage diabetes?
Regular physical activity can improve insulin sensitivity and help control blood sugar levels.
67. How does smoking affect diabetes?
Smoking increases the risk of diabetes complications and should be avoided.
68. Is there a connection between sleep and diabetes?
Poor sleep can affect blood sugar levels and insulin sensitivity, contributing to diabetes management challenges.
69. Can hormonal changes affect diabetes management?
Hormonal changes, such as those during puberty or menopause, can impact blood sugar levels and insulin requirements.
70. What is the role of the pancreas in diabetes?
The pancreas produces insulin and glucagon, hormones crucial for regulating blood sugar levels.
71. What is an insulin pump?
An insulin pump is a device that delivers a continuous supply of insulin to help manage blood sugar levels.
72. Can diabetes affect pregnancy?
Yes, diabetes can impact pregnancy, leading to complications such as gestational diabetes.
73. What is the difference between hyperglycemia and hypoglycemia symptoms?
Hyperglycemia symptoms include increased thirst and frequent urination, while hypoglycemia symptoms involve shakiness and confusion.
74. What is neuropathy in diabetes?
Neuropathy is nerve damage that can occur in diabetes, leading to symptoms like tingling or numbness in the extremities.
75. Can diabetes cause vision problems?
Yes, diabetes can contribute to eye conditions such as diabetic retinopathy.
76. What is the role of a diabetes care team?
A diabetes care team may include endocrinologists, dietitians, nurses, and other healthcare professionals working together to manage diabetes.
77. Can stress management techniques help in diabetes management?
Yes, techniques such as meditation and deep breathing can help manage stress and, in turn, blood sugar levels.
78. What is the relationship between obesity and Type 2 diabetes?
Obesity is a significant risk factor for Type 2 diabetes, and weight management is often part of diabetes prevention and treatment.
79. What is the honeymoon phase in Type 1 diabetes?
The honeymoon phase is a period after the initial diagnosis of Type 1 diabetes when the pancreas may still produce some insulin.
80. Can diabetes affect sexual health?
Diabetes can contribute to sexual health issues, including erectile dysfunction and decreased libido.
81. What is the difference between basal and bolus insulin?
Basal insulin provides a continuous, background level, while bolus insulin is taken before meals to address the immediate rise in blood sugar.
82. How does traveling affect diabetes management?
Traveling can disrupt routine, affecting meal timing and physical activity, requiring adjustments in diabetes management.
83. What is the role of technology in diabetes management?
Technological advancements, such as continuous glucose monitoring (CGM) and insulin pumps, can enhance diabetes management.
84. How does weather impact blood sugar levels?
Extreme temperatures can affect insulin absorption and may require adjustments in diabetes management.
85. What is the Somogyi effect in diabetes?
The Somogyi effect is a rebound phenomenon where hypoglycemia during the night leads to high blood sugar levels in the morning.
86. Is there a link between oral health and diabetes?
Diabetes can contribute to gum disease, emphasizing the importance of good oral hygiene.
87. What is the role of genetics in diabetes risk?
Genetic factors can increase the risk of developing diabetes, especially in Type 2 diabetes.
88. Can stress cause insulin resistance?
Chronic stress may contribute to insulin resistance, impacting blood sugar control.
89. What is insulin sensitivity?
Insulin sensitivity refers to how effectively the body’s cells respond to insulin, influencing blood sugar regulation.
90. How can diabetes affect kidney function?
Diabetes can lead to diabetic nephropathy, a condition that affects the kidneys’ ability to filter blood.
91. What is the role of glucagon in diabetes?
Glucagon is a hormone that raises blood sugar levels by promoting the breakdown of glycogen in the liver.